GLP-1 Agonists and Vision Loss: Examining the Potential Risks
Glucagon-like peptide-1 (GLP-1) agonists have become increasingly popular for managing type 2 diabetes and, more recently, for weight loss. Medications like semaglutide (Ozempic, Wegovy, Rybelsus) and liraglutide (Victoza, Saxenda) have demonstrated significant efficacy in these areas. However, as with any medication, understanding the potential side effects and risks is crucial. Recent discussions and emerging research have raised concerns about a possible link between GLP-1 agonists and vision loss, prompting a closer examination of the available evidence.
This article delves into the current understanding of the relationship between GLP-1 agonists and vision loss. We will explore the mechanisms by which these medications might affect vision, review the existing clinical data, and discuss the importance of informed decision-making when considering GLP-1 agonists. It’s important to note that this article aims to provide information and should not be considered medical advice. Consult with your healthcare provider for personalized guidance.
Understanding GLP-1 Agonists
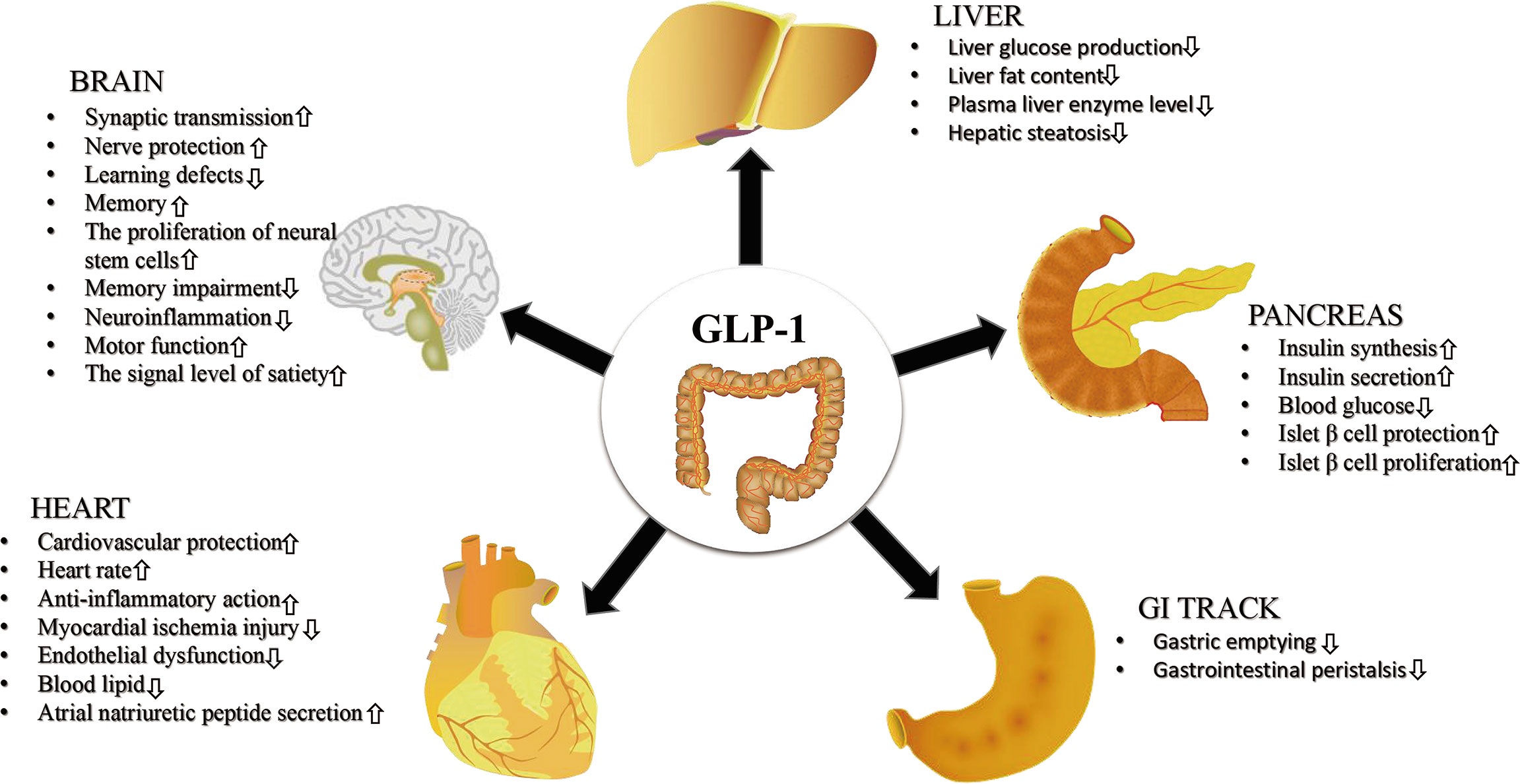
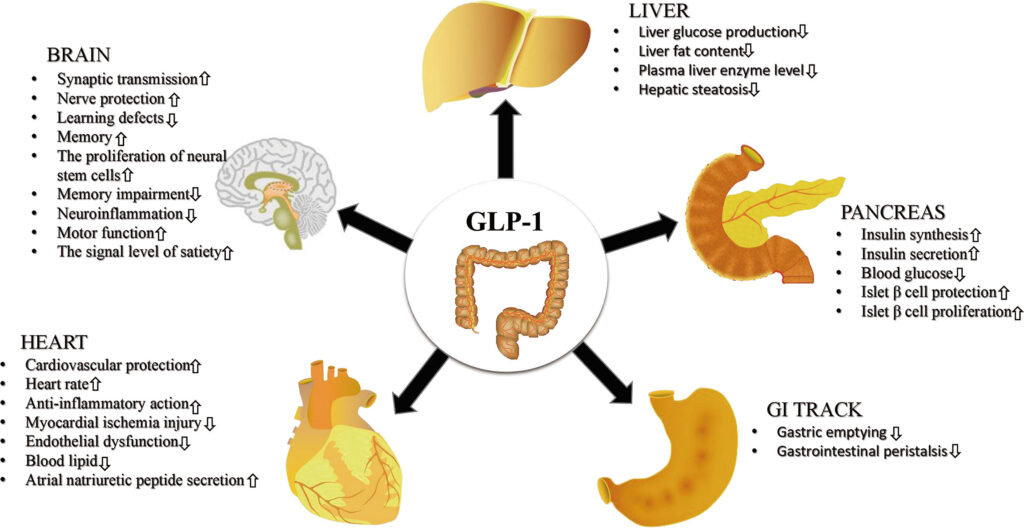
GLP-1 agonists are a class of drugs that mimic the effects of the naturally occurring hormone GLP-1. This hormone plays a vital role in regulating blood sugar levels by stimulating insulin release from the pancreas and reducing glucagon secretion. Additionally, GLP-1 agonists slow down gastric emptying, which contributes to feelings of fullness and can aid in weight loss.
- Mechanism of Action: By mimicking GLP-1, these drugs help lower blood sugar levels after meals and reduce appetite.
- Common Medications: Examples include semaglutide (Ozempic, Wegovy, Rybelsus), liraglutide (Victoza, Saxenda), dulaglutide (Trulicity), and exenatide (Byetta, Bydureon).
- Approved Uses: Primarily used for treating type 2 diabetes and, in some cases, for weight management in individuals with obesity or who are overweight with related health conditions.
Potential Mechanisms Linking GLP-1 Agonists and Vision Loss
While the exact mechanisms are still under investigation, several potential pathways could explain a possible association between GLP-1 agonists and vision loss. It is essential to consider that correlation does not equal causation, and further research is needed to establish a definitive link.
Rapid Blood Sugar Control
One potential mechanism involves the rapid changes in blood sugar levels that can occur when starting or adjusting the dosage of GLP-1 agonists. Fluctuations in blood sugar can affect the lens of the eye, leading to temporary blurring or changes in vision. In some cases, these fluctuations could potentially exacerbate existing eye conditions, particularly in individuals with diabetic retinopathy.
Impact on Diabetic Retinopathy
Diabetic retinopathy, a complication of diabetes, affects the blood vessels in the retina. It’s a leading cause of vision loss in adults. While GLP-1 agonists are designed to improve blood sugar control, which is beneficial for managing diabetic retinopathy in the long term, rapid improvements in blood sugar have, paradoxically, been associated with a temporary worsening of retinopathy in some individuals. This phenomenon is thought to be related to the metabolic stress placed on the retinal blood vessels during periods of rapid glycemic control. [See also: Managing Diabetic Retinopathy with Novel Therapies]
Fluid Retention and Macular Edema
Some studies have suggested that GLP-1 agonists may contribute to fluid retention, which could potentially lead to macular edema, a condition characterized by fluid accumulation in the macula (the central part of the retina). Macular edema can cause blurred vision and distortion. While not a common side effect, it’s a potential concern that warrants further investigation.
Review of Existing Clinical Data
The available clinical data on the relationship between GLP-1 agonists and vision loss is currently limited and somewhat conflicting. Some studies have not found a significant association, while others have reported a possible increased risk of certain eye conditions.
- Clinical Trials: Many large-scale clinical trials evaluating the safety and efficacy of GLP-1 agonists have not identified a significantly increased risk of vision loss or severe eye complications. However, these trials often have specific inclusion and exclusion criteria, and may not fully represent the diverse patient populations who use these medications in real-world settings.
- Post-Market Surveillance: Reports submitted to regulatory agencies, such as the FDA, have included cases of vision loss and eye-related adverse events in individuals taking GLP-1 agonists. However, these reports do not establish a causal relationship and may be influenced by other factors, such as pre-existing eye conditions or other medications.
- Observational Studies: Some observational studies have suggested a possible increased risk of diabetic retinopathy progression in individuals initiating GLP-1 agonist therapy. However, these studies often have limitations, such as confounding variables and difficulties in establishing causality.
The Importance of Informed Decision-Making
Given the current state of knowledge, it is crucial for individuals considering or currently taking GLP-1 agonists to engage in informed decision-making with their healthcare providers. This involves weighing the potential benefits of these medications against the possible risks, including the potential for vision loss or other eye-related complications.
Discuss Your Medical History
Be sure to inform your doctor about any pre-existing eye conditions, such as diabetic retinopathy, glaucoma, or macular degeneration. This information can help your doctor assess your individual risk profile and determine whether GLP-1 agonists are appropriate for you.
Regular Eye Exams
If you are taking GLP-1 agonists, it is essential to undergo regular eye exams by an ophthalmologist or optometrist. These exams can help detect early signs of eye problems and allow for timely intervention if necessary. The frequency of eye exams should be determined in consultation with your eye care provider.
Monitor for Vision Changes
Be vigilant for any changes in your vision, such as blurring, distortion, double vision, or vision loss. Report any such changes to your doctor immediately. Prompt evaluation and treatment can help minimize the potential for permanent vision loss.
Consider Alternative Therapies
If you are concerned about the potential risks of GLP-1 agonists, discuss alternative therapies with your doctor. There are other medications and lifestyle modifications that can help manage type 2 diabetes and promote weight loss. [See also: Lifestyle Changes for Diabetes Management]
Future Research Directions
Further research is needed to clarify the relationship between GLP-1 agonists and vision loss. This research should focus on:
- Large-scale, prospective studies: These studies should be designed to specifically assess the risk of vision loss and other eye complications in individuals taking GLP-1 agonists.
- Mechanistic studies: These studies should investigate the potential mechanisms by which GLP-1 agonists might affect vision.
- Subgroup analyses: These analyses should examine whether certain subgroups of patients (e.g., those with pre-existing eye conditions) are at higher risk of vision loss.
Conclusion
While GLP-1 agonists offer significant benefits for managing type 2 diabetes and promoting weight loss, it is essential to be aware of the potential risks, including the possibility of vision loss. The current evidence is limited and somewhat conflicting, but it is prudent to engage in informed decision-making with your healthcare provider, undergo regular eye exams, and monitor for any changes in your vision. Ongoing research will help to further clarify the relationship between GLP-1 agonists and vision loss and inform clinical practice guidelines.
Always consult with your doctor or other qualified healthcare professional if you have questions about your health or need medical advice. This article is intended for informational purposes only and does not constitute medical advice. The information provided here is not a substitute for professional medical advice, diagnosis, or treatment.