Latent TB Infection Symptoms: Understanding the Silent Threat
Tuberculosis (TB) remains a significant global health concern, affecting millions worldwide. While active TB disease presents with noticeable symptoms, latent TB infection (LTBI) is often asymptomatic, making it a silent threat. Understanding the nuances of latent TB infection symptoms, or rather, the lack thereof, is crucial for effective diagnosis, prevention, and control efforts. This article delves into the characteristics of LTBI, exploring why it’s often called a ‘silent infection’ and the importance of screening and treatment to prevent progression to active TB.
What is Latent TB Infection?
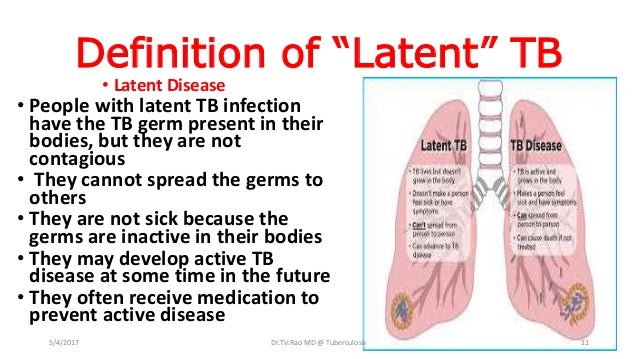
Latent TB infection occurs when a person is infected with Mycobacterium tuberculosis, the bacteria that causes TB, but the immune system is able to contain the infection. In this state, the bacteria remain alive in the body but are inactive. Individuals with LTBI do not feel sick, do not have any symptoms, and cannot spread TB to others. The only indication of infection is a positive result from a TB skin test (TST) or a TB blood test (interferon-gamma release assay, or IGRA). However, without treatment, LTBI can progress to active TB disease, especially if the immune system weakens.
The Absence of Symptoms: Why Latent TB is a Silent Infection
The defining characteristic of latent TB infection symptoms is their absence. Unlike active TB, which manifests with persistent cough, fever, night sweats, weight loss, and fatigue, LTBI presents no outward signs of illness. This lack of symptoms is why LTBI is often described as a ‘silent infection.’ The immune system effectively keeps the bacteria under control, preventing them from causing damage to the lungs or other parts of the body. This makes it difficult to identify infected individuals without specific testing.
Who is at Risk for Latent TB Infection?
Certain populations are at higher risk for contracting Mycobacterium tuberculosis and developing LTBI. These include:
- Close contacts of individuals with active TB disease
- People who have immigrated from countries with high TB prevalence
- Residents and employees of congregate settings such as correctional facilities, homeless shelters, and nursing homes
- Healthcare workers who serve high-risk populations
- People with weakened immune systems, such as those with HIV, diabetes, or undergoing immunosuppressive therapy
- Children exposed to adults at high risk for TB
Diagnosing Latent TB Infection
Since latent TB infection symptoms are non-existent, diagnosis relies on screening tests. The two primary tests used to detect TB infection are:
Tuberculin Skin Test (TST)
The TST, also known as the Mantoux test, involves injecting a small amount of tuberculin under the skin of the forearm. After 48 to 72 hours, a healthcare professional examines the injection site for a raised, hardened area (induration). The size of the induration determines whether the test result is positive, taking into account the individual’s risk factors.
Interferon-Gamma Release Assays (IGRAs)
IGRAs are blood tests that measure the immune system’s response to TB bacteria. These tests are more specific than the TST and are not affected by prior BCG vaccination. IGRAs include QuantiFERON-TB Gold In-Tube (QFT-GIT) and T-SPOT.TB test. They are often preferred for individuals who have received the BCG vaccine or have difficulty returning for a TST reading.
Why Treatment is Crucial for Latent TB Infection
Although individuals with LTBI do not feel sick and cannot spread TB, treatment is essential to prevent the infection from progressing to active TB disease. The risk of progression is highest within the first two years of infection, but it can occur at any time, especially if the immune system becomes compromised. Treatment for LTBI typically involves taking antibiotics for several months. The most commonly used medications include:
- Isoniazid (INH)
- Rifampin (RIF)
- Rifapentine (RPT)
The choice of treatment regimen depends on various factors, including the individual’s age, health status, and potential drug interactions. Adherence to the prescribed treatment is crucial to ensure the eradication of the bacteria and prevent the development of drug-resistant TB. [See also: Tuberculosis Treatment Options]
The Importance of Screening Programs
Given the absence of latent TB infection symptoms, targeted screening programs are vital for identifying and treating individuals at high risk. These programs typically focus on populations with a higher prevalence of TB, such as immigrants from TB-endemic countries, healthcare workers, and people with HIV. Screening involves administering a TST or IGRA, followed by treatment for those with positive results. Effective screening programs can significantly reduce the burden of TB by preventing the progression from latent infection to active disease.
Potential Risks of Untreated Latent TB Infection
While LTBI is asymptomatic, the potential risks of leaving it untreated are significant. The primary concern is the risk of developing active TB disease. Active TB can cause severe damage to the lungs and other organs, leading to serious health complications and even death if left untreated. Additionally, active TB is contagious and can spread to others, perpetuating the cycle of infection. Therefore, identifying and treating LTBI is a critical component of TB control efforts.
Understanding the Progression to Active TB
The progression from latent TB infection to active TB disease occurs when the immune system is no longer able to contain the bacteria. This can happen due to various factors, such as:
- Weakening of the immune system due to HIV infection
- Diabetes
- Kidney disease
- Organ transplantation
- Cancer treatment
- Advanced age
When the immune system weakens, the dormant TB bacteria can reactivate and begin to multiply, causing damage to the lungs and other parts of the body. The symptoms of active TB then become apparent, including cough, fever, night sweats, and weight loss. Early detection and treatment of active TB are crucial to prevent further complications and transmission to others.
Current Research and Future Directions
Ongoing research efforts are focused on developing more effective and shorter treatment regimens for LTBI. Researchers are also exploring new diagnostic tools that can identify individuals at highest risk of progressing to active TB. These advancements hold promise for improving TB control efforts and reducing the global burden of the disease. [See also: New Advances in TB Diagnostics]
The Role of Public Health Initiatives
Public health initiatives play a critical role in TB prevention and control. These initiatives include:
- Raising awareness about TB and LTBI
- Providing access to screening and treatment services
- Implementing infection control measures in healthcare settings
- Conducting surveillance to monitor TB trends
- Collaborating with international organizations to address TB globally
By working together, healthcare professionals, public health officials, and communities can make significant progress in eliminating TB as a public health threat.
Conclusion: Taking Action Against Latent TB
While latent TB infection symptoms are absent, the potential consequences of untreated LTBI are significant. Understanding the risks, getting screened if you are at high risk, and completing treatment if you test positive are crucial steps in protecting your health and preventing the spread of TB. By working together, we can reduce the burden of TB and create a healthier future for all. If you believe you are at risk for latent tuberculosis, contact your healthcare provider to discuss testing and treatment options. Remember, early detection and treatment are key to preventing the progression to active TB and protecting yourself and your community. The absence of latent TB infection symptoms doesn’t mean the absence of risk; it means the need for proactive screening and intervention.
Ultimately, addressing latent TB infection is a shared responsibility. Individuals, healthcare providers, and public health organizations must work together to raise awareness, improve access to care, and ensure that those at risk receive the treatment they need. By taking action against latent TB, we can move closer to a world free of tuberculosis.
