Understanding the Medicaid Fee-for-Service Program: A Comprehensive Guide
The Medicaid program provides essential healthcare coverage to millions of low-income individuals and families across the United States. Among the various models through which Medicaid operates, the Medicaid Fee-for-Service (FFS) program stands out as a traditional approach. This article delves into the intricacies of the Medicaid Fee-for-Service program, exploring its mechanisms, benefits, challenges, and its role within the broader healthcare landscape.
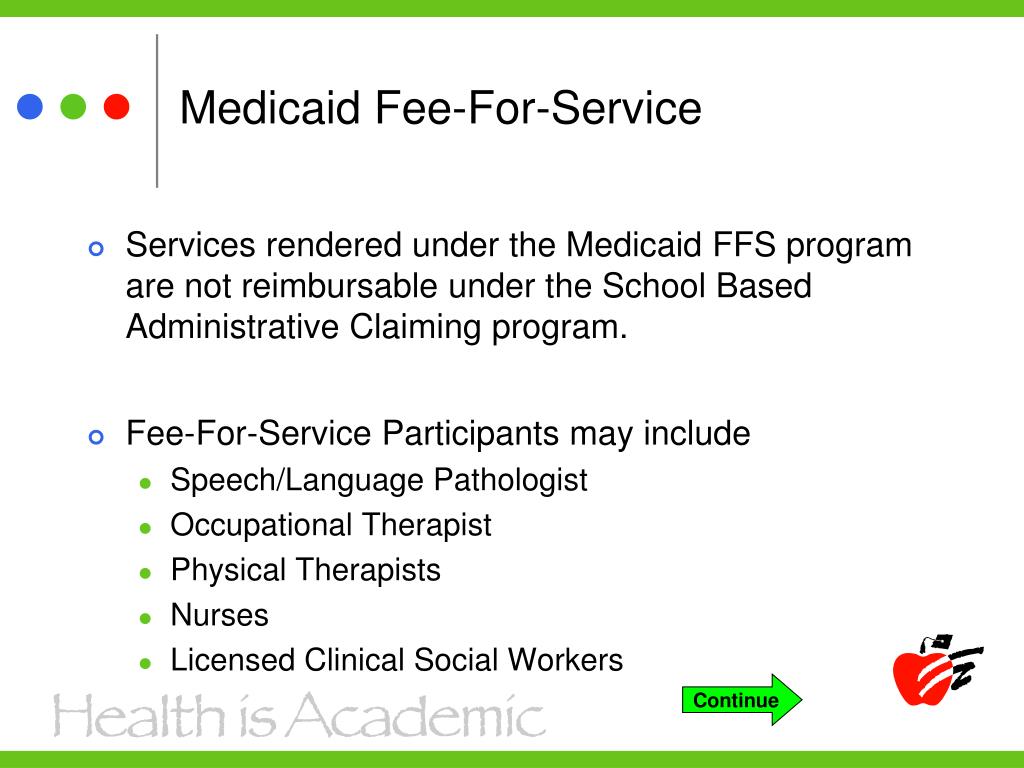
What is the Medicaid Fee-for-Service Program?
The Medicaid Fee-for-Service program is a healthcare payment system where healthcare providers are paid a set fee for each service they render to Medicaid beneficiaries. In this model, the state Medicaid agency or its contracted managed care organizations (MCOs) reimburse providers directly for specific services. This is in contrast to managed care models where providers receive a capitated (per-member, per-month) payment regardless of the volume of services provided.
Under the Medicaid Fee-for-Service program, beneficiaries typically have more freedom in choosing their healthcare providers, as they are not restricted to a specific network. This can be particularly beneficial for individuals with complex medical needs who require specialized care from specific providers.
How the Medicaid Fee-for-Service Program Works
The operational framework of the Medicaid Fee-for-Service program involves several key components:
- Provider Enrollment: Healthcare providers who wish to participate in the Medicaid Fee-for-Service program must enroll with the state Medicaid agency and agree to accept Medicaid’s established fee schedule.
- Service Delivery: Medicaid beneficiaries receive healthcare services from enrolled providers, such as doctor visits, hospital stays, prescription medications, and other medical treatments.
- Claims Submission: Providers submit claims to the Medicaid agency or its designated fiscal agent for each service rendered. These claims include details such as the beneficiary’s information, the specific services provided, and the corresponding billing codes.
- Claims Adjudication: The Medicaid agency reviews the claims to ensure accuracy, compliance with billing guidelines, and medical necessity.
- Reimbursement: If the claim is approved, the provider receives payment according to the established fee schedule. The fee schedule outlines the specific reimbursement rates for each service covered under the Medicaid Fee-for-Service program.
Advantages of the Medicaid Fee-for-Service Program
The Medicaid Fee-for-Service program offers several potential advantages:
- Provider Choice: Beneficiaries generally have greater flexibility in choosing their healthcare providers, as they are not limited to a specific network.
- Transparency: The fee-for-service model provides clear and transparent pricing for individual services, making it easier to track healthcare expenditures.
- Simplicity: The fee-for-service model is relatively straightforward in terms of billing and reimbursement compared to more complex managed care arrangements.
- Access to Specialists: Patients can directly access specialists without needing referrals, facilitating timely and appropriate care.
Disadvantages of the Medicaid Fee-for-Service Program
Despite its advantages, the Medicaid Fee-for-Service program also has several drawbacks:
- Potential for Overutilization: The fee-for-service model may incentivize providers to order more services than necessary, leading to increased healthcare costs.
- Lack of Care Coordination: Without strong care coordination mechanisms, beneficiaries may receive fragmented care from multiple providers, potentially leading to duplication of services and adverse health outcomes.
- Administrative Burden: Providers may face a significant administrative burden in submitting claims and navigating the complexities of Medicaid billing regulations.
- Limited Focus on Prevention: The fee-for-service model may not adequately incentivize preventive care services, as providers are primarily reimbursed for treating illnesses rather than preventing them.
Medicaid Fee-for-Service vs. Managed Care
The Medicaid Fee-for-Service program is often compared to Medicaid managed care, which is another common model for delivering Medicaid services. In managed care, the state contracts with MCOs to provide healthcare services to Medicaid beneficiaries. MCOs receive a capitated payment for each enrollee and are responsible for managing the beneficiary’s care within a network of providers.
Here’s a comparison of the two models:
| Feature | Medicaid Fee-for-Service | Medicaid Managed Care |
|---|---|---|
| Payment Model | Fee-for-each-service | Capitation (per-member, per-month) |
| Provider Choice | Greater flexibility | Limited to network providers |
| Care Coordination | Typically limited | Emphasis on care coordination |
| Cost Control | Potentially less effective | Potential for cost savings |
| Administrative Burden | Can be high for providers | May be lower for providers |
Trends in Medicaid Fee-for-Service Programs
While managed care has become increasingly prevalent in Medicaid, many states continue to operate Medicaid Fee-for-Service programs, either as the primary delivery system or as a supplement to managed care. Several trends are shaping the future of Medicaid Fee-for-Service programs:
- Value-Based Payment: States are increasingly exploring value-based payment models within the Medicaid Fee-for-Service program to incentivize quality and efficiency. These models may include pay-for-performance programs, bundled payments, and shared savings arrangements.
- Care Coordination Initiatives: Many states are implementing care coordination programs within the Medicaid Fee-for-Service program to improve care integration and reduce fragmentation. These programs may involve care managers, health homes, and other strategies to connect beneficiaries with the appropriate services and support.
- Data Analytics: States are using data analytics to identify patterns of overutilization, fraud, and abuse within the Medicaid Fee-for-Service program. This data can be used to target interventions and improve program integrity.
- Telehealth Expansion: The use of telehealth is expanding within the Medicaid Fee-for-Service program, allowing beneficiaries to access healthcare services remotely. This can be particularly beneficial for individuals in rural areas or those with limited mobility.
The Future of Medicaid Fee-for-Service
The Medicaid Fee-for-Service program is likely to remain an important component of the Medicaid landscape, even as managed care continues to grow. States are continually seeking ways to improve the efficiency and effectiveness of Medicaid Fee-for-Service programs through innovations in payment models, care coordination, and data analytics. The key will be to balance the advantages of provider choice and transparency with the need for cost control and care coordination. [See also: Medicaid Managed Care Plans: A State-by-State Comparison]
The ongoing evolution of healthcare delivery and technology will undoubtedly shape the future of the Medicaid Fee-for-Service program. As states strive to provide high-quality, affordable healthcare to their Medicaid populations, the Medicaid Fee-for-Service program will continue to adapt and evolve to meet the changing needs of beneficiaries and providers alike. Understanding the nuances of the Medicaid Fee-for-Service program is crucial for healthcare professionals, policymakers, and anyone involved in the Medicaid system. The program is a vital part of the healthcare safety net, and its continued success is essential for ensuring access to care for vulnerable populations. [See also: Understanding Medicaid Eligibility Requirements]
Ultimately, the goal is to create a Medicaid system that is both efficient and effective, providing beneficiaries with access to the care they need while ensuring responsible stewardship of taxpayer dollars. The Medicaid Fee-for-Service program, with its ongoing adaptations and innovations, will continue to play a significant role in achieving that goal. The evolution of the Medicaid Fee-for-Service program requires constant monitoring and assessment to ensure it aligns with the broader goals of improving health outcomes and reducing healthcare disparities. As healthcare continues to evolve, the Medicaid Fee-for-Service program must adapt to meet new challenges and opportunities.
The Medicaid Fee-for-Service program is a complex and multifaceted system that requires careful attention and ongoing refinement. By understanding its strengths, weaknesses, and evolving trends, stakeholders can work together to ensure that it continues to serve its critical role in providing healthcare access to those who need it most. The Medicaid Fee-for-Service program, despite its challenges, remains a cornerstone of the American healthcare system.
