Navigating the DEA Opioid Training Requirement: A Free Path to Compliance
The Drug Enforcement Administration (DEA) has implemented a new training requirement for all DEA-registered practitioners, addressing the critical need for enhanced knowledge in managing patients with opioid or other substance use disorders. This mandate, effective June 27, 2023, necessitates that practitioners complete a one-time, eight-hour training on substance use disorders, including the appropriate clinical use of all FDA-approved drugs for the treatment of opioid use disorder. Understanding the nuances of this DEA opioid training requirement is crucial for healthcare professionals. Fortunately, several avenues exist for fulfilling this requirement without incurring any cost, offering a free path to compliance.
Understanding the DEA Mandate
The Consolidated Appropriations Act of 2023 brought about this significant change, aiming to equip healthcare providers with the necessary tools and knowledge to combat the opioid crisis effectively. The DEA opioid training requirement applies to all practitioners who are DEA-registered, regardless of their specialty or practice setting. This includes physicians, dentists, physician assistants, nurse practitioners, and other healthcare professionals authorized to prescribe controlled substances.
The rationale behind this mandate is clear: to improve patient safety, reduce opioid misuse, and enhance the quality of care for individuals struggling with substance use disorders. By requiring comprehensive training, the DEA seeks to ensure that practitioners are well-versed in evidence-based practices for pain management, addiction treatment, and the prevention of drug diversion.
Free Options for Meeting the DEA Opioid Training Requirement
While the prospect of an eight-hour training might seem daunting, numerous organizations offer free resources to help practitioners meet the DEA opioid training requirement. These options include:
- Accredited Medical Education Providers: Many medical schools, hospitals, and professional associations offer accredited continuing medical education (CME) courses that fulfill the DEA opioid training requirement. These courses are often available online, allowing practitioners to complete the training at their own pace. Organizations like the American Medical Association (AMA), the American Academy of Family Physicians (AAFP), and the American Society of Addiction Medicine (ASAM) frequently offer free or low-cost training opportunities.
- Government-Sponsored Programs: The Substance Abuse and Mental Health Services Administration (SAMHSA) and the National Institute on Drug Abuse (NIDA) provide a wealth of resources and training materials related to substance use disorders. These agencies often host webinars, workshops, and online courses that meet the DEA opioid training requirement. These resources are typically offered free of charge to healthcare professionals.
- State Medical Boards: Many state medical boards have partnered with educational institutions and professional organizations to offer free training programs that address the DEA opioid training requirement. Check with your state medical board for a list of approved providers and available resources.
- Professional Associations: Various professional associations, such as the American Dental Association (ADA) and the American Association of Nurse Practitioners (AANP), offer continuing education courses that satisfy the DEA opioid training requirement. Membership in these associations may provide access to free or discounted training opportunities.
- DEA-Sponsored Training: The DEA itself provides resources and information on how to comply with the new training requirement. While they may not directly offer eight-hour training courses, they often list approved providers and resources that can help practitioners find free or affordable options.
Key Components of the DEA Opioid Training
The DEA opioid training requirement mandates that the eight-hour training cover specific topics related to substance use disorders. These topics typically include:
- The epidemiology of opioid and other substance use disorders: Understanding the prevalence, risk factors, and consequences of substance use disorders is essential for effective prevention and treatment.
- Pain management strategies: Training should cover evidence-based approaches to pain management, including non-opioid alternatives and multimodal pain management techniques.
- The appropriate clinical use of all FDA-approved drugs for the treatment of opioid use disorder: Practitioners must be knowledgeable about the various medications available for treating opioid use disorder, including their indications, contraindications, and potential side effects.
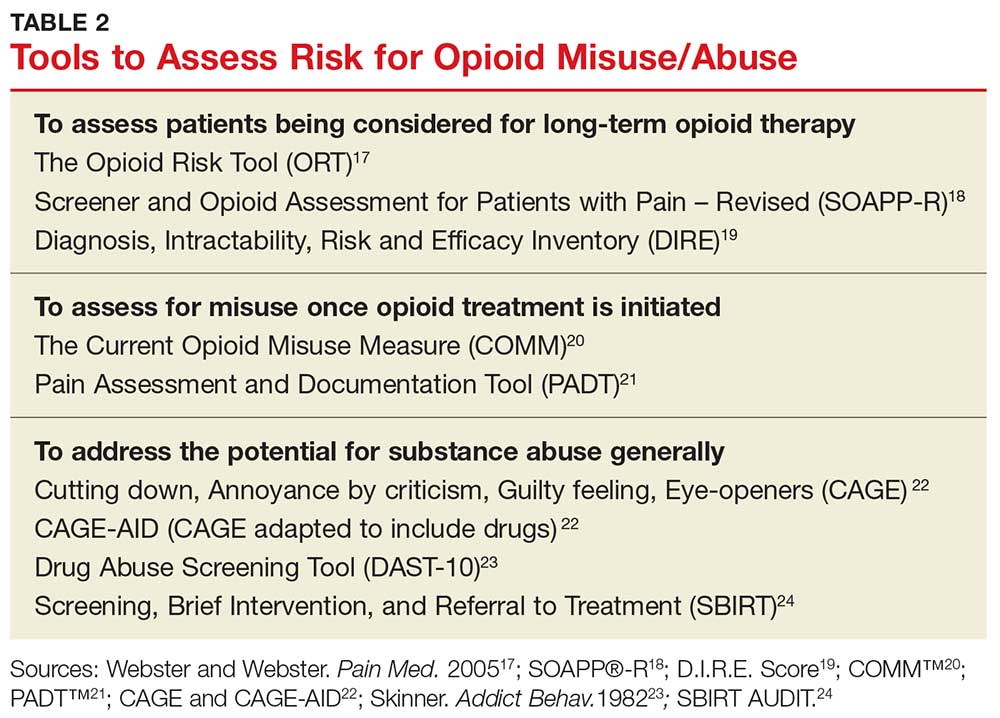
- Recognizing and managing patients with or at risk of developing opioid and other substance use disorders: Training should equip practitioners with the skills to identify individuals who are struggling with substance use disorders or who are at risk of developing these conditions.
- Preventing drug diversion: Practitioners must understand the risks of drug diversion and implement strategies to prevent the misuse and abuse of controlled substances.
- State and federal laws related to controlled substances: A thorough understanding of the legal and regulatory framework governing the prescribing and dispensing of controlled substances is crucial for compliance.
Finding Accredited and Free Training Programs
To ensure that the training you complete meets the DEA opioid training requirement, it is essential to choose an accredited provider. Accreditation signifies that the training program has met rigorous standards for quality and content. Look for programs accredited by organizations such as the Accreditation Council for Continuing Medical Education (ACCME) or the American Osteopathic Association (AOA).
To find free training programs, start by exploring the resources mentioned above, including accredited medical education providers, government-sponsored programs, and state medical boards. Many of these organizations offer online search tools that allow you to filter by topic, accreditation status, and cost. Additionally, consider contacting your professional association or local hospital to inquire about upcoming training opportunities.
The Importance of Ongoing Education
While the DEA opioid training requirement is a one-time mandate, ongoing education and training are crucial for staying up-to-date on the latest advances in addiction treatment and pain management. The field of substance use disorders is constantly evolving, with new research, treatment approaches, and medications emerging regularly. By engaging in continuous learning, practitioners can ensure that they are providing the best possible care to their patients.
Consider attending conferences, workshops, and webinars on substance use disorders to expand your knowledge and skills. Subscribe to professional journals and newsletters to stay informed about the latest research and clinical guidelines. Participate in peer-to-peer learning opportunities to share experiences and learn from your colleagues.
Impact on Patient Care
The DEA opioid training requirement is expected to have a significant positive impact on patient care by improving the knowledge and skills of healthcare professionals in managing patients with opioid or other substance use disorders. By equipping practitioners with the tools they need to prevent, identify, and treat addiction, this mandate has the potential to save lives and improve the quality of life for countless individuals.
Furthermore, the emphasis on pain management strategies and non-opioid alternatives can help to reduce the reliance on opioids for chronic pain, thereby minimizing the risk of addiction and overdose. By promoting evidence-based practices and responsible prescribing habits, the DEA opioid training requirement can contribute to a more rational and effective approach to pain management.
Staying Compliant with the DEA Mandate
To ensure compliance with the DEA opioid training requirement, practitioners must maintain documentation of their completed training. This documentation should include the name of the training provider, the date of completion, the number of hours of training, and a certificate of completion. The DEA may request this documentation during routine inspections or audits.
It is also important to stay informed about any updates or changes to the DEA opioid training requirement. The DEA may modify the training requirements or provide additional guidance on compliance. Regularly check the DEA website and consult with your professional association to stay up-to-date.
Conclusion
The DEA opioid training requirement represents a crucial step forward in addressing the opioid crisis and improving patient care. By providing healthcare professionals with the knowledge and skills they need to manage patients with substance use disorders effectively, this mandate has the potential to save lives and reduce the devastating consequences of addiction. Fortunately, numerous free resources are available to help practitioners meet this requirement and contribute to a healthier, safer community. Embracing these opportunities is not just about compliance; it’s about committing to better patient outcomes and a more responsible approach to pain management.
[See also: Opioid Addiction Treatment Options]
[See also: Understanding Chronic Pain Management]
